Home / Cardiac Output (CO) Monitoring
Cardiac Output (CO) Monitoring
Monitorización del gasto cardíaco (CO)
Monitorización del gasto cardíaco (CO)
El gasto cardíaco (CO) es la cantidad de sangre que se expulsa del corazón por minuto. La monitorización de los componentes del CO en los pacientes es importante para garantizar que exista suficiente volumen de sangre en el cuerpo para transportar oxígeno. Además, la monitorización del CO puede ayudar a los médicos a administrar fluidos, controlar las intervenciones terapéuticas y mejorar los resultados de los pacientes.
La monitorización del CO, junto con otros parámetros hemodinámicos avanzados, se encuentra disponible a través del sistema de monitorización hemodinámica Masimo LiDCO®.
Optimización de fluidos
Optimización de fluidos
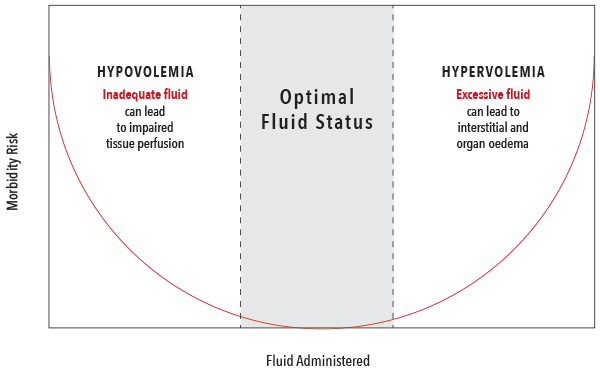
La administración de fluidos es una de las intervenciones más comunes que se realizan para aumentar el CO. Sin embargo, la administración de líquidos debe ser equilibrada para evitar tanto la hipovolemia como la hipervolemia, que se han asociado con resultados negativos.1
Componentes del suministro de oxígeno
Componentes del suministro de oxígeno
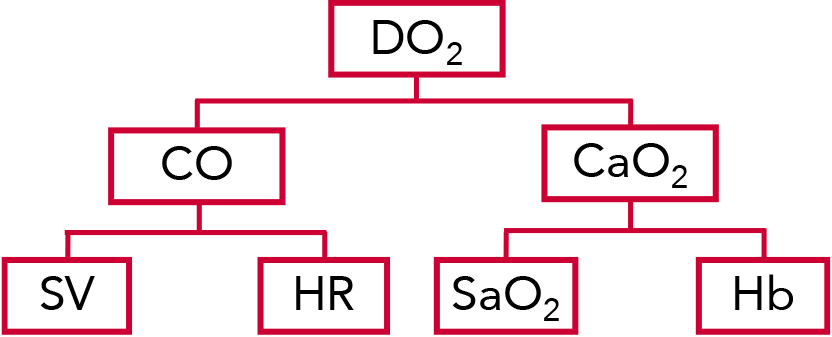
El suministro de oxígeno (DO2) es la cantidad de oxígeno que se proporciona a los tejidos, calculada como el producto del CO y el contenido de oxígeno (CaO2).3
El CO se calcula multiplicando el volumen sistólico (SV) por la frecuencia cardíaca (HR) del paciente. El SV es la cantidad de sangre que bombea el ventrículo izquierdo del corazón en una contracción.3
El DO2 y el CaO2 están influenciados por la saturación de oxígeno (SaO2) y la hemoglobina (Hb) del paciente.3
Parámetros normales de hemodinámica4-8
| Parámetro | Ecuación | Frecuencia normal |
| Suministro de oxígeno (DO2) | CaO2 x CO x 10 | 950‑1150 ml/min |
|---|---|---|
| Gasto cardíaco (CO) | HR x SV/1000 | 4,0‑8,0 l/min |
| Contenido de oxígeno (CaO2) | (0,0138 x Hgb x SaO2) + (0,0031 x PaO2) | 17‑20 ml/dl |
| Volumen sistólico (SV) | N/A | 60‑100 ml/latido |
| Saturación de oxígeno (SaO2) | N/A | 95 – 100% |
| Hemoglobina total (Hb) | N/A | Hombres: 13,8‑17,2 g/dl Mujeres: 12,1‑15,1 g/dl |
| Frecuencia cardíaca (HR) | N/A | La frecuencia varía según el estado del paciente (en reposo frente a activo, edad, etc.) |
Descripción general de la tecnología del algoritmo PulseCO™
Descripción general de la tecnología del algoritmo PulseCO™
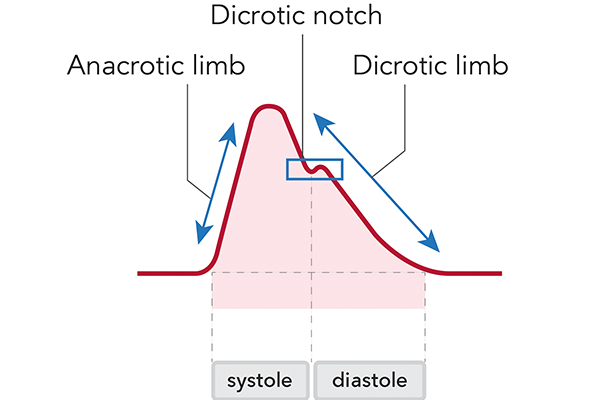
El algoritmo PulseCO proporciona un CO y un SV continuos latido a latido mediante el análisis de una forma de onda de presión sanguínea. El algoritmo se basa en principios físicos y fisiológicos, y se centra en el análisis de la potencia del pulso en lugar de en la forma o el contorno de la forma de onda. A diferencia de otros algoritmos de presión arterial, PulseCO no se basa en estadísticas, ni en suposiciones sobre la distensibilidad vascular, ni en la detección de la muesca dicrótica, que suele ser un reto con las señales arteriales periféricas. Como resultado, el algoritmo PulseCO evita las limitaciones de otras tecnologías de monitorización hemodinámica basadas en la presión del pulso o en contornos.
El estándar de oro actual en la monitorización hemodinámica, aunque no se usa tan comúnmente debido a su invasividad, es el catéter de la arteria pulmonar (CAP). El algoritmo PulseCO se ha validado frente al CAP, lo que demuestra una buena concordancia entre los dos métodos.9
Evidencia clínica de PulseCO
Evidencia clínica de PulseCO
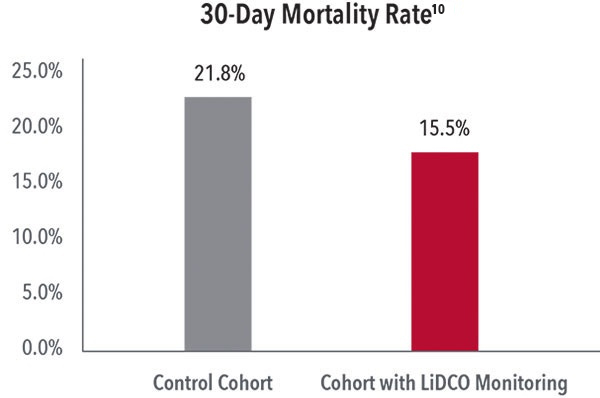
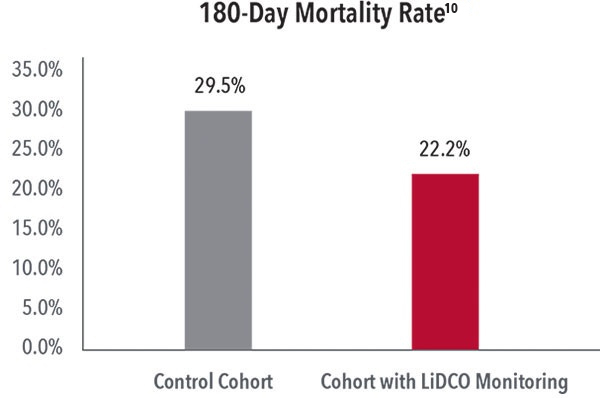
Reducción de la mortalidad a los 30 días y a los 180 días
En un estudio en el que se compararon los resultados de 600 pacientes sometidos a una laparotomía de emergencia, los investigadores comprobaron que, tras la implementación de un programa que incluía la monitorización de LiDCO con la tecnología PulseCO, se produjo una reducción de la mortalidad a los 30 días (del 21,8 al 15,5 %) y a los 180 días (del 29,5 al 22,2 %).10
Reducción de costes y complicaciones posoperatorios
En un ensayo controlado aleatorizado de 743 pacientes sometidos a una cirugía abdominal mayor, los investigadores comprobaron que la optimización hemodinámica con la monitorización de LiDCO con la tecnología PulseCO dio lugar a una reducción del 20 % de las complicaciones posoperatorias, lo cual supuso un ahorro medio de 530 $ en el tratamiento de los pacientes monitorizados con la monitorización de LiDCO con la tecnología PulseCO en comparación con los pacientes de control que no fueron monitorizados.1
Cartera de productos de Masimo LiDCO
RECURSOS
PLCO-007127/PLM-14934A-0724 EN-PLM-13198A